What is Genetic Testing or Screening?
Genetic Testing is the direct examination of one’s DNA to identify specific gene mutations (mistakes) that are known to lead to diseases like Batten, Cystic Fibrosis, Muscular Dystrophy and others.
Why is Genetic Testing important?
Genetic testing plays a critical role in accurately diagnosing diseases early enough to prevent an all too common time-consuming, expensive and emotionally exhausting diagnostic odyssey, to prevent treatment errors resulting from misdiagnoses, and to ensure patients and their families receive the support and educational services they need.7,13 Genetic testing can also be useful in family planning following the birth of an affected child.
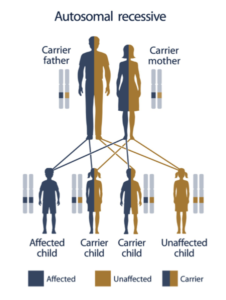
What does it mean to be a “carrier?”
Normally, every person has two copies of every gene, one inherited from each parent. Many (but not all) genetic diseases require two defective genes in order to develop; if one inherits one normal and one mutated gene, he or she does not have the disease but is a carrier and can pass the mutated gene onto their children (Autosomal Recessive).
Why screen for rare diseases? They’re rare and don’t affect many people.
While the incidence of each individual rare disease is low, these numbers add up: an estimated 25-30 million people in the United States are afflicted with one of more than 6,800 rare diseases, 80% of which are genetic. The worldwide incidence is estimated to be 350 million people – more than AIDS and cancer combined.11
Why screen for rare diseases for which no treatment is available?
In order to bring a drug to market for any disease, the U.S. FDA requires proof of concept studies in reliable animal models of the disease, valid comparisons between animal models and affected patients, and well-defined methods for assessing individual treatment responses. Without properly diagnosed patient pools to study, none of these criteria can be met inhibiting drug development.
The History of Genetic Screening
Newborn screening began in the 1960s when Dr, Robert Guthrie developed a blood test for newborns that could detect phenylketonuria (PKU), a condition which leaves infants unable to break down the amino acid phenylalanine, causing serious symptoms like seizures and mental retardation.8 Fortunately, PKU is treatable with a restricted diet.
The first large-scale carrier screening came in the early 1970s, a time when 1 in 158 infants born on the island of Cyprus were at risk for beta thalassemia, a life-threatening blood disorder. To address this issue, the government and Orthodox Church established a policy of mandatory carrier screening and counseling prior to starting a family.2 As a result, the disease has virtually disappeared from the Island.1
Rabbi Joseph Eckstein pioneered a similar program offering genetic screening to members of the Jewish community to eliminate Tay-Sachs and other genetic disorders common in the Jewish community. One in 27 Ashkenazi Jews are carriers for Tay-Sachs, but incidence in North America has dropped 90% since the start of the screening program.5,6,9
The Current State of Genetic Testing
Since the start of newborn screening for PKU, scientists have developed more tests to screen newborns for up to 60 different disorders. 6 However, states vary in the number (30-60), types of conditions, and quality of their testing protocols.
Carrier screening is available for more than 60 of the estimated 5,200 rare genetic diseases, but individual tests can range from $200 to $1,200; making comprehensive preconception carrier screening cost-prohibitive for even the wealthiest families.6,12 Importantly, most affected infants are from families with no history of the disorder, so making carrier screenings more widely accessible is key to reducing the incidences of these genetic disorders
